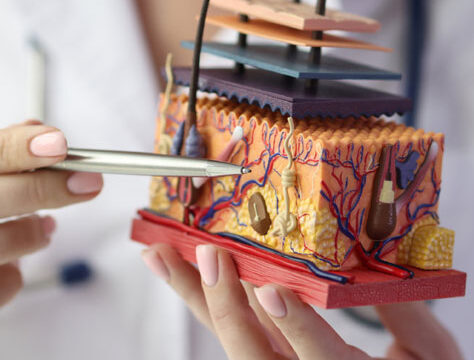
Wound healing isn’t just a natural response—it’s a complex biological process influenced by numerous factors. For wound care nurses, understanding how chronic health conditions interfere with wound recovery is essential for delivering the best patient outcomes.
In this blog, we’ll explore the impact of chronic diseases like diabetes, heart disorders, obesity, and autoimmune diseases on wound healing—and offer practical strategies you can implement right away.
Diabetes mellitus is one of the leading causes of delayed wound healing worldwide. Persistently high blood sugar damages blood vessels and nerves, reducing circulation and sensation—especially in the feet. This leads to slow-healing wounds, often unnoticed until complications like ulcers or infections develop.
Monitor blood sugar regularly and encourage tight glycemic control.
Educate patients on daily foot inspections and proper footwear.
Use moist wound healing dressings and timely debridement to speed recovery.
Heart-related conditions like hypertension, peripheral artery disease (PAD), and congestive heart failure (CHF) can significantly restrict blood flow to wound sites. Reduced oxygenation means slower healing and higher risk of infections or chronic ulcers.
Elevate limbs to manage swelling and reduce pressure.
Encourage smoking cessation and healthy lifestyle habits.
Coordinate with cardiologists to ensure optimal circulation support.
Obesity increases inflammation and decreases blood flow to wound areas. Excess body fat also puts added mechanical stress on pressure points, making healing even more difficult—especially after surgeries or with pressure ulcers.
Check for signs of poor tissue perfusion regularly.
Advocate for nutritional support, especially high-protein diets.
Use offloading devices and pressure redistribution tools.
Conditions like lupus, rheumatoid arthritis, and multiple sclerosis often result in systemic inflammation and a weakened immune response. Many patients are also on immunosuppressants, further delaying wound recovery.
Monitor wounds for subtle signs of infection.
Work closely with the care team to balance medication and wound care.
Consider advanced therapies like negative pressure wound therapy (NPWT) when healing stalls.
Chronic conditions present major hurdles in wound healing, but with knowledge, vigilance, and the right interventions, wound care nurses can make a real difference.
By focusing on patient education, collaborative care, and condition-specific wound management, you can prevent complications, accelerate healing, and enhance overall patient wellbeing.
Learn more about Crescent Wound Care’s very own wound care certification program by visiting:
Certification